Alimentary System
Esophagus - Hyperkeratosis
Narrative
Hyperkeratosis in the absence of hyperplasia has interpretative implications different from those of hyperkeratosis occurring as part of the process of enhanced epithelial proliferation. In the anorectic rodent, the excess keratin is presumably the result of reduced mechanical removal by the passage of food. In cases of hyperkeratosis in the esophagus associated with anorexia, hyperkeratosis is usually also present in the forestomach. In these situations, there will be no evidence of an increased proliferative response in the basal layer. Alternatively, vitamin imbalance and zinc deficiency can cause parakeratotic hyperkeratosis and associated squamous cell hyperplasia.
Bertram TA, Markovits JE, Juliana MM. 1996. Non-proliferative lesions of the alimentary canal in rats GI-1. In Guides for Toxicologic Pathology. STP/ARP/AFIP, Washington, DC, 1-16.
Full Text: https://www.toxpath.org/docs/SSNDC/GINonproliferativeRat.pdfHargis AM, Ginn PE. 2007. The integument. In: Pathologic Basis of Veterinary Disease, 4th ed (McGavin MD, Zachary JF, eds). Mosby, St Louis, MO, 1107-1261.
National Toxicology Program. 2010. NTP TR-544. Toxicology and Carcinogenesis Studies of Dibromoacetonitrile (CAS No. 3252-43-5) in F344/N Rats and B6C3F1 Mice (Drinking Water Studies). NTP, Research Triangle Park, NC.
Abstract: https://ntp.niehs.nih.gov/go/32617National Toxicology Program.1993. NTP TR-400. Toxicology and Carcinogenesis Studies of 2,3-Dibromo-1-propanol (CAS No. 96-13-9) in F344/N Rats and B6C3F1 Mice (Dermal Studies). NTP, Research Triangle Park, NC.
Abstract: https://ntp.niehs.nih.gov/go/12251Sigler RE, Dominick MA, McGuire EJ. 1992. Subacute toxicity of a hydroxymethyl glutaryl-coenzyme A deductase inhibitor in Wistar rats. Toxicol Pathol 20:595-602.
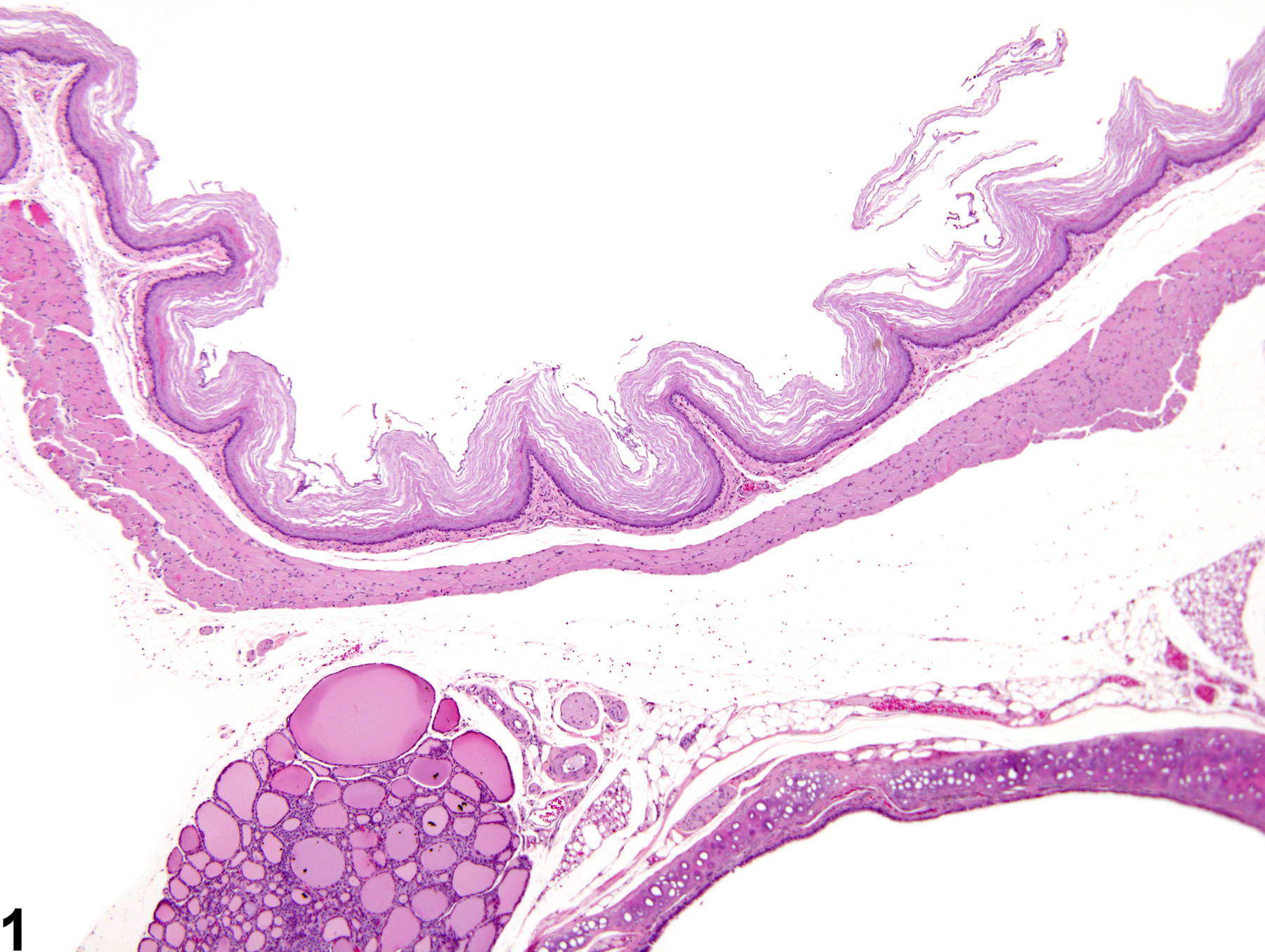
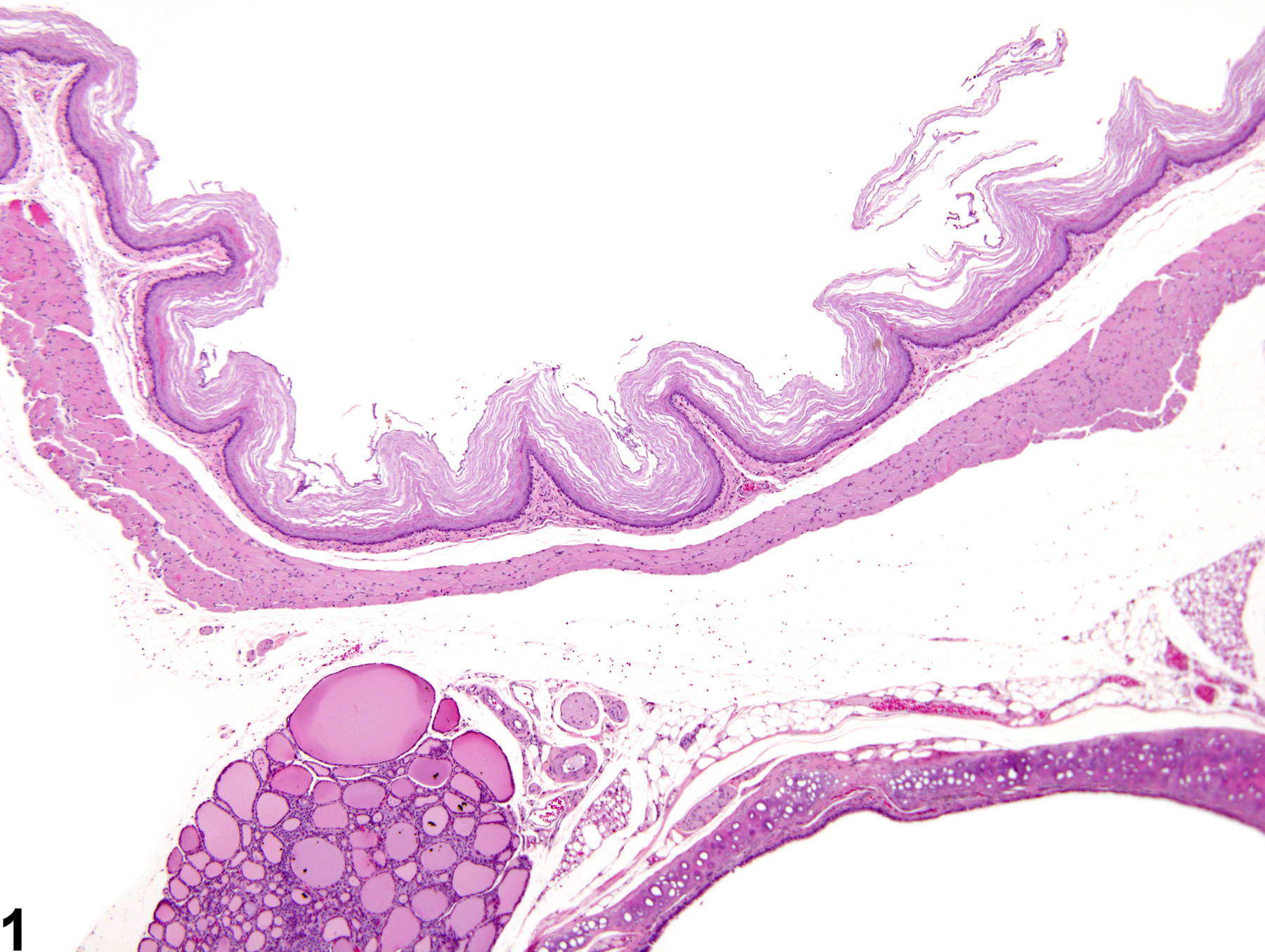
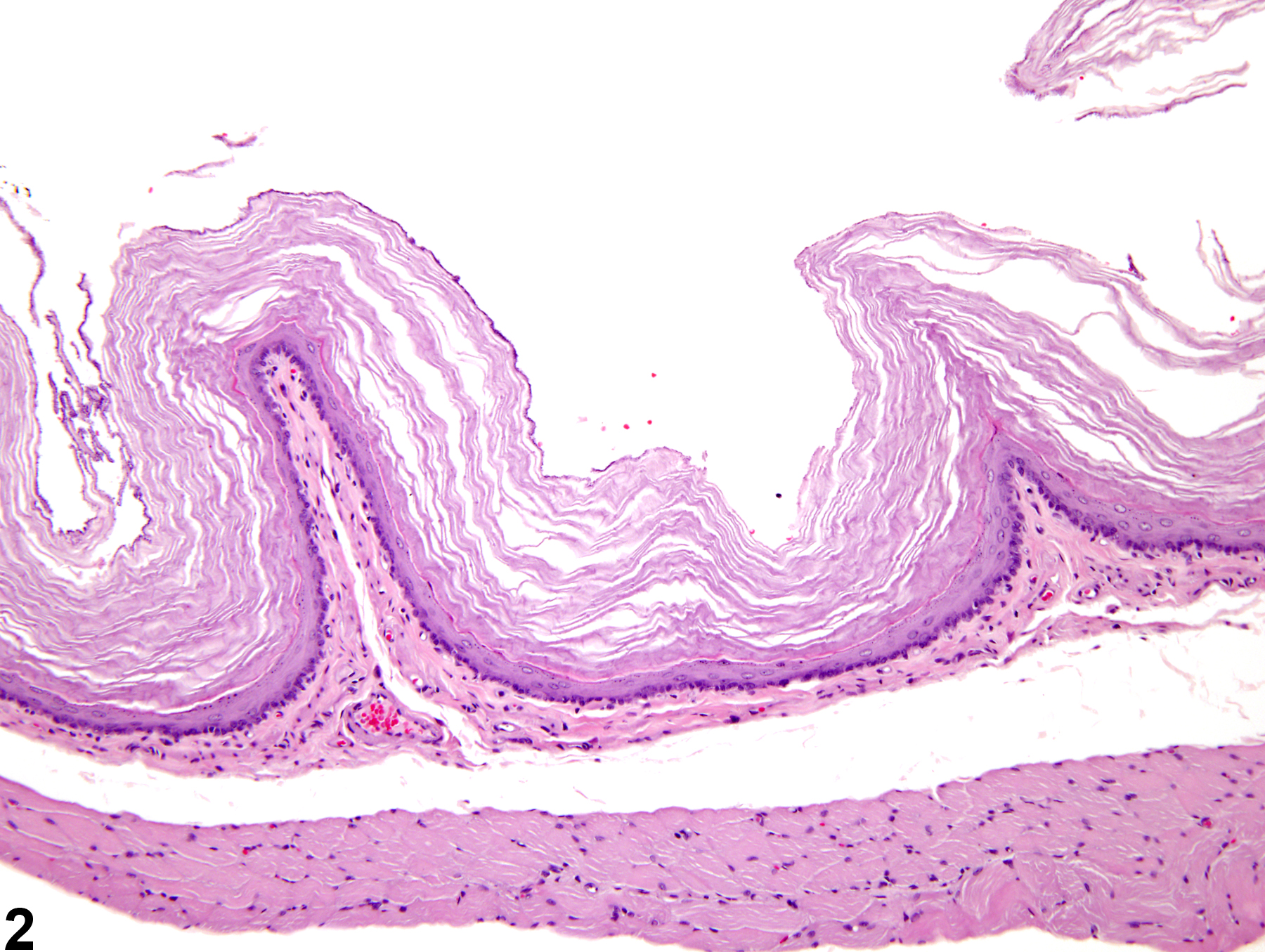
Esophagus - Hyperkeratosis in a female F344/N rat from a chronic study. There are excess, anuclear keratin layers on the surface of the epithelium.